Understanding Homocysteine: What It Is and Why It Matters
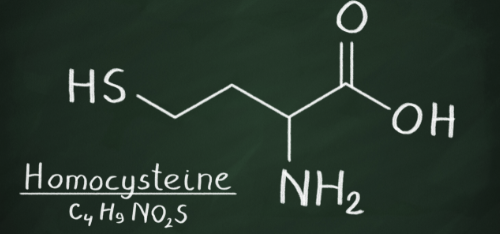
Homocysteine is a naturally occurring amino acid in your blood. It is produced when your body processes the essential amino acid methionine (from dietary protein) through a normal metabolic pathway.
Under normal conditions your body either:
converts homocysteine back into methionine (requires adequate levels of certain B-vitamins such as folate/B9 and B12), or
converts homocysteine into other harmless compounds via an alternate pathway, depending on nutrient status and enzyme function.
When homocysteine levels become abnormally high, a condition called Hyperhomocysteinemia, this reflects a potential disruption in these metabolic pathways.
High homocysteine matters because it is correlated with increased risk of cardiovascular disease. Elevated homocysteine can contribute to oxidative stress and may damage the structural integrity of blood vessel walls.
Why High Homocysteine Often Means Problems with B-Vitamins or Methylation
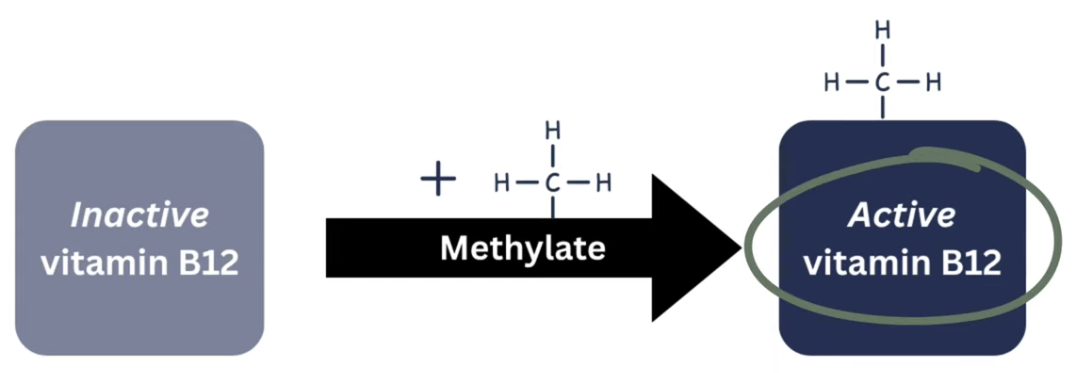
When homocysteine stays elevated, it often signals a deficiency or impaired use of B-vitamins (especially folate (B9) or B12) because those vitamins are required for the methylation process that converts homocysteine back into methionine.
In other words, elevated homocysteine can mean either you are not getting enough of these nutrients through diet, or your body is struggling to “activate” or “methylate” them properly so they can do their job.
This is why we care about homocysteine: it can serve as a sensitive metabolic marker telling us something important about your B-vitamin status, methylation capacity, and cardiovascular risk, even if standard annual bloodwork did not reveal anything.
The Case for Testing Homocysteine + B-Vitamins (Rather Than Guessing)
Most routine annual panels do not measure homocysteine levels. That means many people may have underlying elevated homocysteine and increased risk without knowing it. At Gutwell Medical we always include homocysteine in our panels because it gives clinically valuable insight.
When we test homocysteine, we also test serum B12 and folate. If homocysteine is high and B-vitamins are low or suboptimal, that points toward a likely nutritional or absorption deficiency. If vitamins are adequate but homocysteine remains high, that suggests a problem with methylation or metabolic processing perhaps due to genetic variants or impaired enzyme function.
This is far more precise than guessing based on symptoms or dietary recall.
MTHFR: What It Is, How it Relates to Homocysteine, and Why It Is Not the Whole Story
The MTHFR gene encodes an enzyme (methylenetetrahydrofolate reductase) that is essential in folate metabolism. It converts folate into its active form (5-MTHF), which is required for the re-methylation of homocysteine back into methionine.
There are two genes that are best studied with relation to MTHFR, and estimates suggest that 60–70% of individuals may carry at least one variation in these genes.
The effect of these variants on the enzyme’s function depends on how many copies someone has (heterozygous - 1 copy vs homozygous - 2 copies) and which variant(s). The number of copies, and which gene they are on will determine how well the MTHFR enzyme functions. Some variations may lead to up to 70% less enzyme activity, while others might only be 25-35% less.
Because these variants are common and many people with them remain healthy, having one does not automatically mean you need high doses of methylated vitamins or that you necessarily have increased risk of heart disease. The presence of a variant simply means your methylation pathway may be less efficient and you might benefit from tailored nutrition or support - but context matters.
We cannot rely on genotype alone. That is why functional testing (homocysteine, B12, folate, methylation markers) gives us a clearer, individualized picture.
Why Methylation Matters: Beyond Homocysteine
Methylation involves adding a methyl group (1 carbon and 3 hydrogens) to a molecule. It influences:
DNA methylation and gene expression (epigenetics)
Neurotransmitter production and brain chemistry
Detoxification pathways and antioxidant defenses
Cellular repair, membrane stability, hormone metabolism
When methylation is impaired, the downstream effects may include elevated homocysteine, impaired detoxification, oxidative stress, and increased risk of chronic disease. That is why supporting methylation, when needed, is a central focus in functional nutrition.
How to Get Natural Methyl Donors From Food
While supplements can be helpful for people with elevated homocysteine or methylation challenges (more on that below), food is a great foundation to start with. Many whole foods provide natural methyl donors or support the biochemical pathways that keep homocysteine in a healthy range. Focusing on these foods can gently strengthen methylation without relying solely on supplements.
Foods Rich in Folate (Natural Vitamin B9)
Folate is one of the most important nutrients for converting homocysteine back into methionine. Natural folate is especially valuable because it is already in a form your body can use.
Dark leafy greens such as spinach, chard, collard greens, romaine
Asparagus
Avocado
Lentils and black beans
Broccoli and Brussels sprouts
Citrus fruits
Foods High in Vitamin B12
Vitamin B12 is essential for the remethylation pathway. It is found naturally in:
Salmon and sardines
Eggs
Grass fed beef
Poultry
Dairy products
For vegans, B12 needs to come from fortified foods or supplementation since plant foods do not contain reliable B12.
Foods Rich in Choline
Choline provides methyl groups through the betaine/homocysteine pathway. It also supports liver function and brain health.
Eggs, especially the yolks
Salmon
Chicken and turkey
Grass fed beef
Brussels sprouts and broccoli
Peanuts
Foods That Provide Betaine (Trimethylglycine)
Betaine is a direct methyl donor that helps lower homocysteine through the alternate transsulfuration pathway.
Beets and beet juice
Spinach
Quinoa
Wheat bran or wheat germ
Shellfish
Magnesium Rich Foods
Magnesium supports many enzymes involved in methylation.
Pumpkin seeds
Almonds and cashews
Black beans
Swiss chard and spinach
Whole grains
Avocado
Putting It All Together
A nutrient dense, whole foods diet naturally delivers many of the methyl donors needed to keep homocysteine in a healthy range. The ideal pattern includes leafy greens, high quality proteins, eggs, legumes, beets, and a wide variety of vegetables. This is a gentle and sustainable approach to supporting methylation.
A Practical, Nuanced Approach: Testing First, Then Personalized Nutrition or Support
Because of all this complexity: we do not simply assume someone “has MTHFR” and start megadosing methylated B-vitamins. Instead, we test homocysteine, B-vitamin levels (B12, folate), and sometimes MTHFR genotype, then interpret results in context. If homocysteine is elevated and vitamins are low or low-normal, first-line approach is to correct deficiencies with appropriate B-vitamin supplementation.
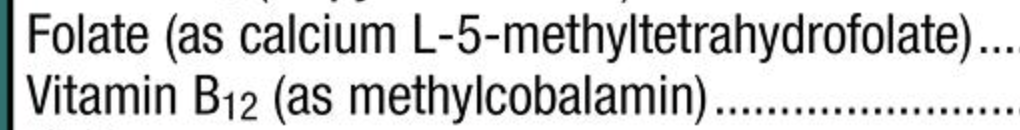
Methylated Vitamins
When looking at vitamins, if you see folate listed as L-5-methyltetrahydrofolate or 5-MTHF and vitamin B12 listed as methylcobalamin as seen on the right - those are the methylated forms. Vitamins with these forms are generally more expensive than forms like cyanocobalamin (B12) and folic acid (folate), which are the inactive forms.
If homocysteine is high despite adequate B-vitamins, or if there are other methylation-related symptoms, more in-depth evaluation of methylation pathways may be called for.
This individualized strategy of testing first, then supporting as needed reduces guesswork and improves safety and efficacy.
Why Homocysteine Screening Is Important in Preventive Nutrition and Functional Medicine
Because high homocysteine is a modifiable risk factor and often linked with vitamin status or methylation capacity, screening for it gives people a real opportunity to intervene early. Correcting elevated homocysteine through nutrition or targeted supplementation can help reduce long-term cardiovascular risk and support overall metabolic health.
As a functional nutritionist I believe this is a powerful tool for early detection and prevention, especially in people with family history of heart disease, metabolic issues, or unexplained symptoms such as fatigue, neurological complaints, or poor detox capacity.