The Migrating Motor Complex: A Missing Link in IBS and Digestive Symptoms
If you have been struggling with chronic bloating, nausea, early fullness, abdominal discomfort, or irregular bowel habits, you may have been told you have Irritable Bowel Syndrome (IBS). Many patients come to me after years of symptoms, multiple tests, and trial-and-error treatments without lasting relief. One of the most overlooked root causes of IBS-like symptoms is a disruption in something called the Migrating Motor Complex, often abbreviated as the MMC.
Understanding the migrating motor complex can completely shift how we think about chronic digestive symptoms and can open the door to treatment approaches that help the gut heal rather than simply suppressing symptoms.
In this article, we will explore what the migrating motor complex is, how it relates to IBS, and what you can do to support healthy digestive motility.
Where My Perspective Comes From
Before transitioning into functional gastroenterology, I spent more than 25 years in a traditional GI practice where we had many referrals for motility disorders and complex IBS cases. During that time, I began noticing patterns. Many patients with nausea, bloating, early satiety, and irregular bowel habits were given different diagnoses, but their symptoms seemed to stem from the same underlying issue. When I shifted toward addressing gut motility and the microbiome, I started to see patients experience lasting improvements.
This journey led me to place major clinical focus on the migrating motor complex.
Functional Dyspepsia, Gastroparesis, and SIBO: Overlapping Symptoms, Different Names
Patients often come into the clinic with symptoms such as bloating, gas, abdominal pain, early satiety, nausea, constipation, or diarrhea. These symptoms appear in several overlapping conditions.
Functional Dyspepsia
A disorder involving discomfort in the upper abdomen without structural abnormalities seen on imaging or endoscopy.
Common symptoms: bloating, upper abdominal discomfort, early fullness, belching, nausea.
Gastroparesis
Gastroparesis refers to delayed stomach emptying, often caused by nerve or muscle abnormalities in the stomach.
Common symptoms: bloating, nausea, vomiting, early fullness, abdominal discomfort, and sometimes constipation.
SIBO, SIFO, and IMO
These are overgrowths of bacteria, fungus/yeast, or methane-producing microbes in the small intestine. These are named according to what species are overgrown: SIBO = small intestinal bacterial overgrowth, SIFO = small intestinal fungal overgrowth, and IMO = intestinal methanogen overgrowth.
For SIBO, there can be an overgrowth of bacteria that produce hydrogen, methane, or hydrogen sulfide gases. Hyrdogen sulfide is more newly understood, and Dr. Pimentel has developed a test called the TrioSmart that we use in our office, which is able to detect all 3 gases (hydrogen, methane, hydrogen sulfide).
SIFO is intestinal fungal overgrowth, which is a Candida overgrowth in the small bowe (small intestine).
Common symptoms: bloating, gas, abdominal pain, early fullness, diarrhea or constipation.
Why It Is Hard to Distinguish Between These Conditions
The symptoms overlap significantly. The difference is where the issue originates:
Functional dyspepsia and gastroparesis are related to abnormalities in the stomach.
SIBO, SIFO, and IMO refer to overgrowths in the small intestine.
A thorough history is vital. I spend 90 minutes with new patients to understand where in the GI tract symptoms occur, what triggers them, and how they have evolved. This helps identify the correct root cause and an effective treatment plan.
Why Standard Gastric Emptying Tests Are Limited
Gastroparesis is traditionally diagnosed using a gastric emptying scan, where the patient eats a low-fat, low-fiber radiolabeled meal and imaging shows how quickly it empties. However:
The test meal (egg whites, toast, jam) is not representative of real meals as it does not contain any significant fat or fiber.
Circadian rhythms can change results.
Many patients I scoped after overnight fasting still had visible food, often plant fiber, remaining in the stomach, even when their gastric emptying test was read as normal. This suggests a functional delay that the test did not capture.
New research now shows that functional dyspepsia and gastroparesis exist on a spectrum, not as distinct conditions. In fact, up to 37% of patients diagnosed with functional dyspepsia actually have delayed gastric emptying.
This brings us back to the migrating motor complex.
What Is the Migrating Motor Complex?
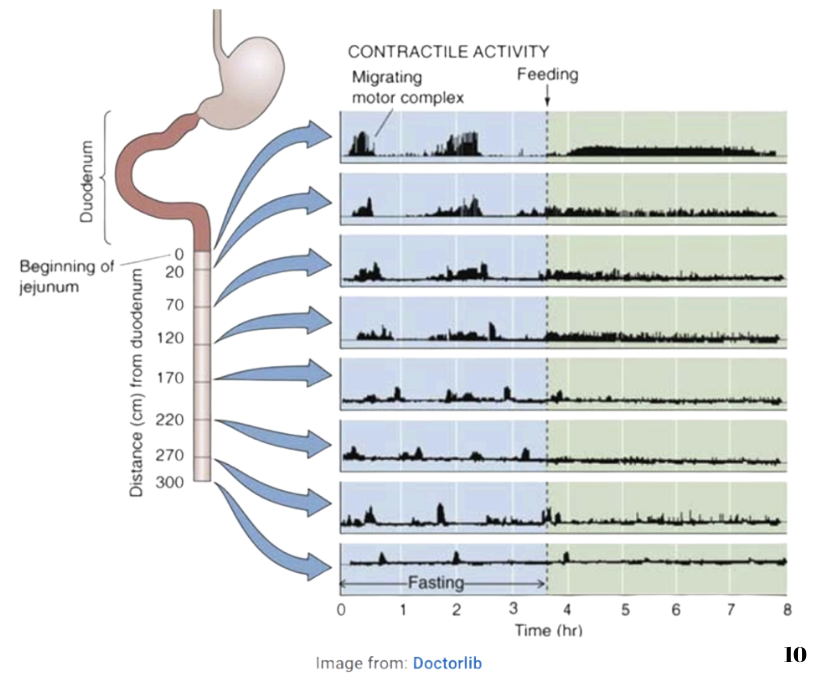
The Migrating Motor Complex (MMC) is a powerful electrical wave of muscular contractions that sweeps through the stomach and small intestine when we are not eating. It acts like the gut’s self-cleaning cycle. Its job is to move food particles, debris, bacteria, and toxins through and out of the small intestine.
Key points about the MMC:
It begins when the stomach is completely empty.
It requires at least 90 minutes of digestive rest to activate.
Eating (generally anything over 200 calories) stops the MMC.
Fat delays MMC activation the longest, while protein delays it the least.
MMC function is essential for preventing bacterial overgrowth.
When the MMC is impaired, food and debris sit longer than they should. This can result in:
Bloating and fullness
Fermentation of food in the small intestine
Microbial overgrowth and dysbiosis
Nausea and reduced appetite
Gas and discomfort after small meals
This is where IBS-like symptoms often begin.
MMC Function and the Microbiome
Supporting the MMC is one of the most effective ways to maintain a balanced microbiome, because the MMC prevents stagnant material from collecting in the small intestine, where it can fuel microbial overgrowth.
As a reminder, the gut microbiome is the community of trillions of microorganisms that live inside the digestive tract. These organisms help with digestion, immune regulation, nutrient absorption, and maintaining the intestinal lining.
A healthy microbiome functions like a lush rainforest. The more diverse the environment, the more resilient it is. Different species balance and support one another.
When stress, illness, processed foods, or antibiotics disturb the microbiome, it becomes less diverse. This is similar to seeing brown patches appear in a rainforest. As diversity declines, digestion becomes less efficient, inflammation increases, and symptoms like bloating and early satiety become more likely.
Why Traditional Gastroparesis Diets Often Fall Short
Conventional diets for gastroparesis focus on symptom avoidance and minimizing digestive discomfort. While they can provide short-term relief, they do not nourish or restore the microbiome and they do not address the root cause of impaired motility.
Our goal is restoration and long-term healing, not symptom suppression.
Restoring and Optimizing the Migrating Motor Complex
Once I recognized the central role of the MMC in digestive health, I developed a structured nutritional and lifestyle approach that supports healthy gastric emptying and restores proper MMC function. The key goals are:
Allow the stomach to fully empty.
Reduce mechanical workload on the stomach.
Strengthen and nourish the gut microbiome.
This protocol is designed not just to reduce symptoms, but to help the gastrointestinal tract regain its natural rhythm.
1. Smoothie-Based Nutrition
Whole plant foods contain fibers that require strong muscular grinding in the stomach. When gastric motility is impaired, these fibers may remain in the stomach overnight and prevent the MMC from activating.
Smoothies empty primarily by gravity rather than mechanical churning, which means:
The stomach can empty more fully
The MMC has an opportunity to activate naturally
The small intestine receives nutrients without heavy digestive strain
The smoothies I use are intentionally therapeutic. They typically include:
Berries rich in phytonutrients and prebiotics that support microbiome diversity
Goat milk and goat milk kefir, which provide easily digestible fats, prebiotics, and probiotics
An anti-inflammatory gut-healing powder to support intestinal lining repair
This not only improves motility but also nourishes the microbiome and supports long-term healing.
2. Removing Inflammatory Foods
Inflammatory foods can irritate the intestinal lining and interfere with both motility and microbiome balance. Removing these foods allows the stomach and small intestine to heal, decreasing symptoms and improving digestive function.
3. Ensuring the Stomach is Empty Before Bed
Having the stomach empty at bedtime allows the MMC to sweep the small intestine overnight. This is a key part of preventing bacterial overgrowth and maintaining a balanced microbiome.
4. Supporting Nervous System Calm
The brain and digestive system communicate constantly. Stress, hypervigilance, and chronic worry can inhibit gastric motility. Clear structure, nervous system soothing practices, and creating predictable eating rhythms help restore normal digestive signaling.
5. Targeted Supplements and Testing When Needed
Some patients also benefit from additional evaluation to identify microbial imbalance, enzyme deficiency, or other contributing factors. Supplements are used strategically to further support healing.
Conditions Successfully Supported Using This Approach
This method has shown clinical benefit for patients with:
IBS
SIBO, SIFO, and IMO
Functional dyspepsia
Gastroparesis
C. difficile infection
Microscopic colitis
Diverticulitis flare recovery
Crohn’s disease
Post-infectious digestive symptoms
Every treatment plan is individualized, but the principles remain the same: support motility, nourish the gut lining, and restore microbial balance.
You Do Not Have to Live with Chronic Digestive Symptoms
If you have been told everything looks “normal” on tests, but your symptoms are very real, there may be an explanation that has not yet been considered.
To learn more or schedule a consultation, reach out to us today. We are here to help you understand your symptoms, restore your digestion, and feel like yourself again.
References:
ALKaisy QH, Al-Saadi JS, Al-Rikabi AKJ, Altemimi AB, Hesarinejad MA, Abedelmaksoud TG. Exploring the health benefits and functional properties of goat milk proteins. Food Sci Nutr. 2023;11(10):5641-5656. Published 2023 Jun 27. doi:10.1002/fsn3.3531”
American Gastroenterological Association technical review on the diagnosis and treatment of gastroparesis. Parkman, Henry P. et al. Gastroenterology, Volume 127, Issue 5, 1592 - 1622
Approaches to increase the gastric residence time: Floating drug delivery systems- A review - Scientific Figure on ResearchGate. Available from: https://www.researchgate.net/figure/nterdigestive-Myloelectric-Cycle-or-Migrating-Myloelectric-Cycle-MMC-FACTORS-AFFECTING_fig1_247774737 [accessed 23 Jul 2025]
Baek GH, Kim YJ, Lee Y, Jung SC, Seo HW, Kim JS. Prebiotic potential of green banana flour: impact on gut microbiota modulation and microbial metabolic activity in a murine model. Front Nutr. 2023;10:1249358. Published 2023 Oct 31. doi:10.3389/fnut.2023.1249358
Cleveland Clinic. Gastroparesis diet. Cleveland Clinic. https://my.clevelandclinic.org/-/scassets/files/org/digestive/gastroparesis-clinic/gastroparesis-diet Accessed July 27, 2025.
Egboh SM, Duncanson K, Potter M, Keely S, Talley NJ. Functional dyspepsia and gastroparesis: are they distinct disorders, a spectrum of diseases or one disease?. eGastroenterology. 2025;3(1):e100119. Published 2025 Jan 23. doi:10.1136/egastro-2024-100119
Kalt W, Cassidy A, Howard LR, et al. Recent Research on the Health Benefits of Blueberries and Their Anthocyanins. Adv Nutr. 2020;11(2):224-236. doi:10.1093/advances/nmz065
Kellow JE, Borody TJ, Phillips SF, et al. Human interdigestive motility: variations in patterns from esophagus to colon. Gastroenterology. 1986;91:386–395.
La Torre C, Caputo P, Cione E, Fazio A. Comparing Nutritional Values and Bioactivity of Kefir from Different Types of Animal Milk. Molecules. 2024;29(11):2710. Published 2024 Jun 6. doi:10.3390/molecules29112710
Lavefve L , Howard LR , Carbonero F . Berry polyphenol metabolism and impact on human gut microbiota and health. Food Funct. 2020;11(1):45-65. doi:10.1039/c9fo01634a
Pimentel M, Soffer EE, Chow EJ, Kong Y, Lin HC. Lower frequency of MMC is found in IBS subjects with abnormal lactulose breath test, suggesting bacterial overgrowth. Dig Dis Sci. 2002;47(12):2639-2643. doi:10.1023/a:102103903241
Sanger GJ, Hellström PM, Näslund E. The hungry stomach: physiology, disease, and drug development opportunities. Front Pharmacol. 2011;1:145. Published 2011 Feb 18. doi:10.3389/fphar.2010.00145
Sarna S. K. (1985). Cyclic motor activity; migrating motor complex: 1985. Gastroenterology 89, 894–913
Takahashi T. Interdigestive migrating motor complex -its mechanism and clinical importance. J Smooth Muscle Res. 2013;49:99-111. doi:10.1540/jsmr.49.99
Vantrappen G, Janssens J, Peeters TL (November 1981). "The migrating motor complex". The Medical Clinics of North America. 65 (6): 1311–29. doi:10.1016/S0025-7125(16)31474-2. PMID 7035768.)
Wang C, Fang X. Inflammation and Overlap of Irritable Bowel Syndrome and Functional Dyspepsia. J Neurogastroenterol Motil. 2021;27(2):153-164. doi:10.5056/jnm20175
Wauters L, Ceulemans M, Schol J, Farré R, Tack J and Vanuytsel T (2022) The Role of Leaky Gut in Functional Dyspepsia. Front. Neurosci. 16:851012. doi: 10.3389/fnins.2022.851012